Abstract
Introduction: HIT is a relatively common and potentially catastrophic prothrombotic disorder caused by platelet activating antibodies targeting complexes of platelet factor 4 (PF4) and heparin. Diagnosis rests on clinical features coupled with serologic assays, most commonly an ELISA for heparin-PF4 antibodies. The ELISA optical density (OD) is a surrogate for antibody titer, an OD < 1 conveying a likelihood for pathogenic platelet-activating antibodies of < 1%, while OD > 2.0 confirms clinically suspected platelet activating antibodies in about 90%. The treatment for HIT is alternative anticoagulation, effecting platelet recovery >100,000 usually within 3 days and in the great majority within 7 days. We and others have observed very delayed platelet recovery (sometimes for weeks; "persisting HIT") and this appeared more common with high titer antibodies. We did a retrospective analysis of 116 patients with HIT from single institution to investigate whether high titres of antibodies in HIT is associated with prolong time to platelet recovery and its potential impact on overall survival.
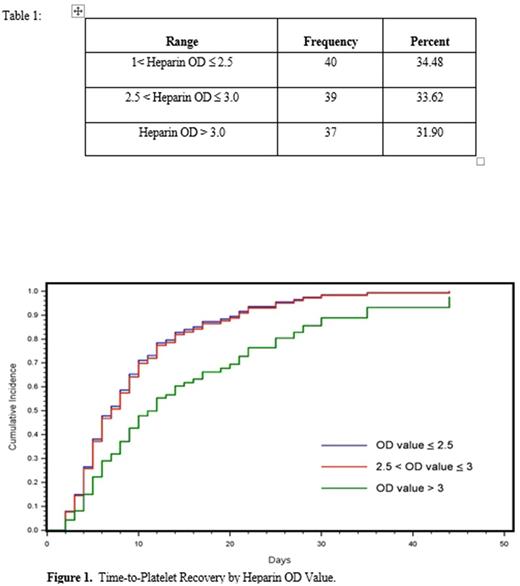
Method: We retrospectively reviewed 116 patients diagnosed with HIT in our institution from 2009 to 2017 using our hospital database. Charts were reviewed for clinical comorbidities, association of surgery, thromboembolic events, type of alternative anticoagulation used on HIT diagnosis, platelet nadir count and time to recovery, and the relationship to ELISA OD. For statistical analysis, patients with HIT were categorized into 3 cohorts based on OD 1 to OD equal or less than 2.5, OD 2.5 to OD equal or less than 3 and OD more than 3 (Table 1). Patients with OD less than or equal to 2.5 was chosen as the reference group. A competing risk analysis based on the Fine & Gray method investigated differences in cumulative incidence of platelet recovery among the cohorts. Death before recovery was treated as a competing risk. Pooled t- test analysis was used to study correlation between OD and survival.
Results: Median age of 116 patients was 65 years (63-68 ; 95% CI). 60.3% of the patients were male. Median value of initial platelet count during admission was 212k. Median value of nadir platelet count after diagnosis of HIT was 47k. 90% had surgery prior to diagnosis of HITT. 57% of patients with HIT had thromboembolic disease. 53%; 15% and 9% of patients were transitioned to Coumadin, NOACs and Arixtra respectively after initially getting treated with alternative anticoagulation Bivalirudin for HIT. Out of 116 patients, 101 patients (87%) of patients had platelet recovery in median of 6 days. The heparin OD value is significantly different between the two cohorts (p=0.0485) based on a pooled t-test. We further categorized all the patients into 3 cohorts based on their PF4 OD to study its impact on time to platelet recovery as shown in Table 1.There was no significant difference in recovery time between patients with OD between 2.5 and 3.0 and those less than 2.5 (p = 0.7207). The estimated hazard ratio of 0.921 [95% CI: (0.588, 1.444)], implying that patients with a higher OD value were likely to take slightly longer to recover their platelet count. However there was a statistically significant difference in platelet recovery time for patients OD greater than 3.0 (p = 0.0260) with hazard ratio 0.598 [95% CI: (0.380, 0.940)] compared to the reference group (see Figure 1). In-hospital mortality was 24.14% (28 patients) but was not significantly different by ELISA OD (p=0.7432). There is ongoing analysis of relationship of ELISA OD to thrombotic complications.
Conclusion: Time to platelet recovery was significantly increased in HIT patients with heparin-PF4 OD value > 3. The lack of impact on overall survival probably relates to the fact that most deaths with HIT are related to underlying disorders (multiorgan failure, severe cardiac disease, cancer) rather than complications of HIT per se. A larger prospective study might further clarify the impact of PF4 OD on HIT treatment and outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal